By Pankaj Dhaka and J.S. Bedi
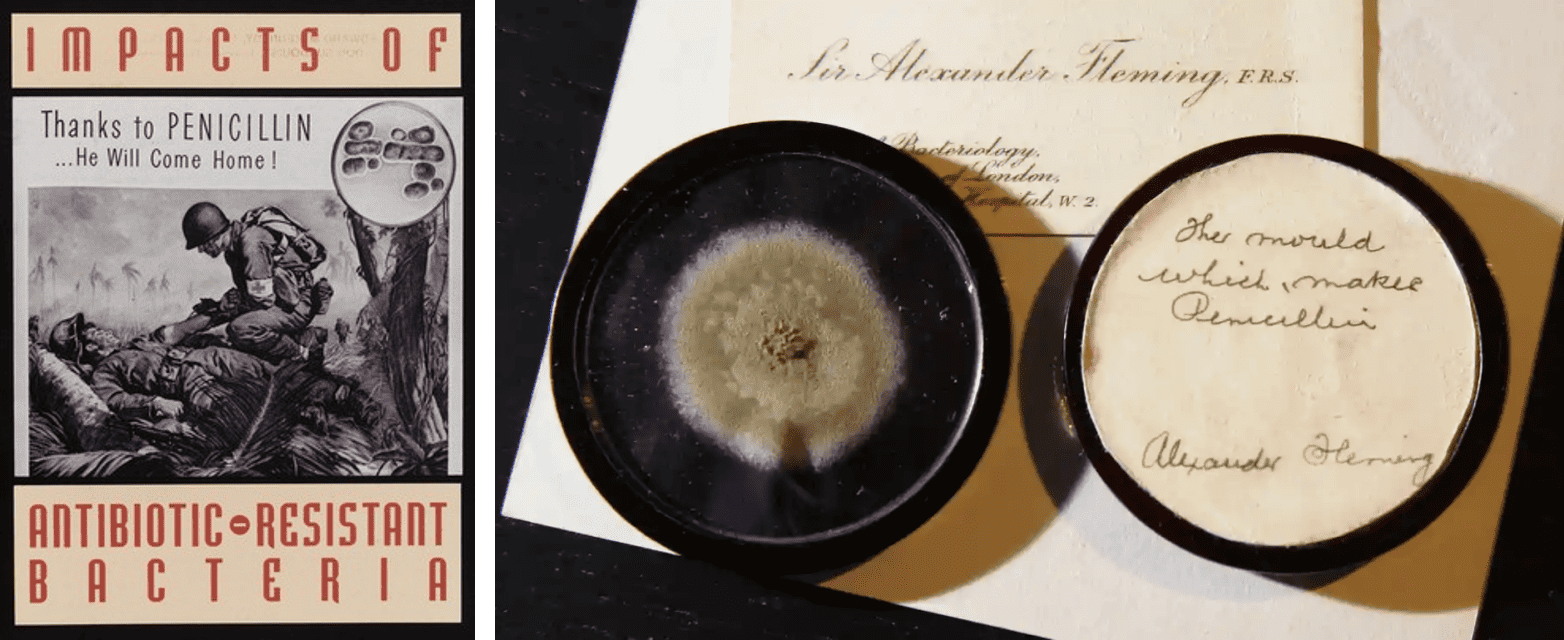
The discovery of the antibiotic Penicillin by Alexander Fleming in the year 1928 spawned the antibiotics era in the infectious disease treatment paradigm, wherein experts rightly described antibiotics as a “miracle drug”. The world before the discovery of antibiotics was so vulnerable to infections that even a minor cut or injury could lead to death. Upon the commercial production and marketing of antibiotics in the 1940s, antibiotics saved millions of infection-related deaths across the globe. It would not be incorrect to say that antibiotics greatly underpin the success of modern medicine, saving millions of lives as it finds use in the treatment and prevention of blood-related infections, infectious miscarriages, infections after Cesarean sections, urinary tract infections, infections after surgeries, as well as in cancer treatments and organ transplantation. Similarly, antibiotics have also played an important role in the advancement of the animal husbandry sector, where these drugs have been commonly used as therapeutics (for treatment), prophylactic (for disease prevention), and as growth promoters.

Soon after the arrival of antibiotics on the market, scientists and health experts, including Fleming, had warned about the consequences of irresponsible use (e.g., underuse, prophylactic use, or overuse) of these ‘miracle drugs’ in the form of ‘acquired antibiotic resistance’ in bacteria. Antimicrobial resistance (AMR) is a broader term for biological resistance to antimicrobials in different types of microorganisms, including bacteria.
When a given antimicrobial doesn’t work for a particular infection, the physician often switches over to another, more potent, antimicrobial agent. This, sometimes, has increased side effects and also prolongs the course of treatment. At times, the causative microorganism fails to respond to any of the antimicrobials used for the treatment. Unfortunately, we don’t have many antimicrobials in our arsenal, to begin with, and the emergence of resistant and stronger microorganisms (also known as ‘superbugs’) puts us in a vulnerable state.
Microorganisms gain resistance against antimicrobials that are used to kill them as part of their natural evolution. Currently, many of the microorganisms, largely bacteria, that cause serious infections have gained resistance to most of the readily used antimicrobials making our worst nightmares a reality. Imagine a time when none of the available antimicrobial drugs works against infections. Unfortunately, this is proving to be true for some of the infections where the highest level of antimicrobials are also not effective in treating them.
Why do microorganisms become resistant to antimicrobials?
Microorganisms, such as bacteria, have been around on earth for about 3.8 billion years, a timeframe that allowed them to acquire the needed biological weaponry to combat various environmental stressors including antibiotics. Antibiotics not only eliminate some of the infection-causing bacteria but also force some bacteria to mutate and acquire resistance to that antibiotic. Some multiply fast (in minutes), making thousands of copies and each round of multiplication allows them to mutate their genetic material to adapt to the persistent external threats to survive. The antibiotic resistant-survivor bacteria sustain themselves during the antibiotic treatment. These mutant bacteria or superbugs then pass over the mutated genetic material to their progeny or to a neighbouring bacteria, and within a short period, the antibiotic-resistant gene passes through an entire bacterial population. All the bacteria, consequently, become resistant to the antibiotic treatment.
AMR is one such natural phenomenon that bacteria and other microorganisms use to defend themselves against various survival or selection pressures existing in the environment, including that of antimicrobials. Both good and bad (disease-causing) microorganisms rely on the phenomenon of AMR to protect themselves. So while AMR is a naturally occurring phenomenon in all microorganisms, human actions are accelerating this process in disease-causing bacteria and other pathogens at a much more rapid pace due to large scale and frequent antibiotic or more broadly, antimicrobial misuse.
The growing problem of AMR
A recent study reported that antibiotic-resistant bacterial infections were responsible for 1.27 million deaths in 2019 (approx. 3500 individuals per day), and this is expected to jump to 10 million a year by 2050 if we don’t address the AMR crisis urgently and effectively. Further, in developing nations, AMR is associated with huge socio-economic losses as drug-resistant infections require patients to spend more time in hospitals which eventually increases the treatment costs as well as the risk of mortality. This also puts tremendous pressure on the health systems and food security.
In many countries, antibiotic stewardship programmes (guidelines for proper usage of antibiotics) in hospital settings are not adequately formulated or implemented which leads to the improper prescription of antibiotics by medical professionals. In countries like India, people are able to buy antibiotics over-the-counter which contributes to irresponsible antibiotic use. Furthermore, poor sanitation and hygiene practices in home, community and healthcare settings add to the burden of infectious diseases, including hospital-acquired infections. In such a scenario, lack of awareness about AMR is often the reason behind the misuse of these life-saving drugs.
In addition to the antimicrobial misuse in the human health sector, the agriculture, livestock, poultry and aquaculture sectors are major drivers of AMR. In fact, nearly three-quarters of all antibiotics sold each year is used on factory farms. The use of antimicrobials as prophylaxis or growth promoters to compensate for poor farm practices lead to AMR in bacteria/microorganisms associated with farm animals. This sub-concentration of drug doses can exert the selection pressure on the microbes to mutate in favour of acquiring drug resistance. These resistant bacteria or superbugs may spill over to humans either directly (e.g., animal handling) or indirectly through the environment (e.g., through animal foods or the environment in the form of animal manure to crops) and other possible routes.
Moreover, due to the rise of AMR, we are already running out of effective drugs for many of the existing infections (e.g., multidrug-resistant tuberculosis, urinary tract infections, sepsis cases in newborns, etc.). On the other hand, the development of a new drug requires huge financial investments, collaborations among stakeholders and rigorous clinical trials. There is also no guarantee of its effectiveness in the long run which means the pathogens can eventually acquire resistance to these new drugs too.
What can we do to address the problem of AMR?
The good news is that there’s a lot we can do to stop the spread of drug-resistant infections. In addition to using antibiotics judiciously, we should focus on infection prevention strategies such as hand washing, proper food safety, access to clean water, effective hygiene and sanitation of the environment, and adherence to vaccination schedules for vaccine-preventable diseases, etc. We must try to rear farm animals and pets under good biosecurity measures so that reliance on antibiotics can be reduced by minimizing the chances of infections. Additionally, we need to use antibiotics carefully and sensibly (e.g., don’t take antibiotics for flu or other viral diseases!). So, it is important to avoid the over-the-counter purchase of antibiotics, always consult the physician, and not force them to prescribe antibiotics. Pharmaceutical companies manufacturing antibiotics and related products should dispose them off responsibly. Like other public health issues, social awareness of AMR is crucial and we need a robust campaign to make people aware of the problem of AMR in our country and help them understand the severity of this ongoing but a rarely talked about health crisis. Many are unknowingly contributing to the problem of AMR.
‘Resistance anywhere is resistance everywhere’ Centers for Disease Control and Prevention (CDC). As we saw in the case of COVID-19, viruses or superbugs don’t recognise borders, age, race, and economic status. It is also important to acknowledge that the issue of AMR impacts human, animal, and environmental health similarly considering they are interconnected. It is this understanding that forms the basis of the ‘One Health’ approach to tackling AMR. As described by the CDC “One Health is a collaborative, multisectoral, and transdisciplinary approach — working at the local, regional, national, and global levels — with the goal of achieving optimal health outcomes recognizing the interconnection between people, animals, plants, and their shared environment”. The human and animal health sectors share many of the common classes of antibiotics for the treatment of infectious diseases. As a result, the resistant bugs arising either in humans, animals or their environment may spread from one component to the other. Therefore, the issue of AMR must be tackled through the participation of various stakeholders in different sectors within the framework of One Health.

Authors, Pankaj Dhaka and J.S. Bedi are researchers based at the Centre for One Health, Guru Angad Dev Veterinary and Animal Sciences University, Ludhiana, Punjab, India. Pankaj is the recipient of the Superheroes Against Superbugs Fellowship. As part of the Fellowship, Pankaj is organising AMR awareness workshops at schools in the state of Punjab. The SaS team (Renu, Sarah and Somdatta) provided inputs for the article.
References and further reading:
- Murray, C.J., Ikuta, K.S., Sharara, F., Swetschinski, L., Aguilar, G.R., Gray, A., Han, C., Bisignano, C., Rao, P., Wool, E. and Johnson, S.C., 2022. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. January 2022
- O’Neill, J. Antimicrobial Resistance: Tackling a crisis for the health and wealth of nations. London: Review on Antimicrobial Resistance. Review on Antimicrobial Resistance. December 2014
- One Health Basics by Centers for Disease Control and Prevention, 2022.